Introduction to Mitral Regurgitation
Definition and Causes
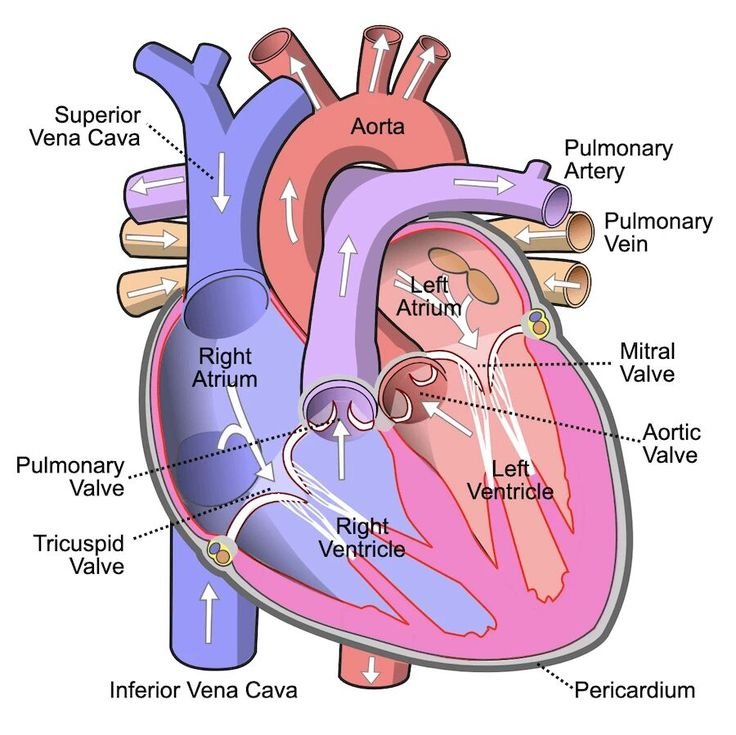
Mitral regurgitation occurs when the heart’s mitral valve does not close tightly, causing blood to flow backward in the heart. This can lead to various causes, including heart conditions like mitral valve prolapse, heart attack, or infections affecting the valve. Other factors such as age-related changes, rheumatic fever, or congenital heart defects can also contribute to this condition.
Symptoms and Diagnosis
Symptoms of mitral regurgitation may not always be present, but when they do occur, they can include fatigue, shortness of breath, irregular heartbeat, or swelling in the ankles. Diagnosis often involves a physical exam, imaging tests like echocardiograms, and possibly other diagnostic procedures to assess the severity and underlying cause of the condition. Early detection and management of mitral regurgitation are crucial to prevent complications and improve the quality of life for affected individuals.
Types of Mitral Regurgitation
Acute Mitral Regurgitation
Acute mitral regurgitation is a sudden onset of severe backflow of blood due to a malfunction in the mitral valve. This condition can be caused by factors such as a heart attack, infective endocarditis, or trauma to the heart. Patients with acute mitral regurgitation may experience symptoms like chest pain, rapid heart rate, and severe shortness of breath. Prompt medical intervention is crucial to prevent life-threatening complications and preserve heart function.
Chronic Mitral Regurgitation
Chronic mitral regurgitation involves a gradual deterioration of the mitral valve over time, leading to ongoing leakage of blood backward in the heart. This type of regurgitation can be caused by conditions like mitral valve prolapse, rheumatic heart disease, or degenerative changes in the valve structure. Patients with chronic mitral regurgitation may develop symptoms gradually, including fatigue, heart palpitations, and difficulty breathing, especially during physical activity. Regular monitoring and management strategies are essential to prevent further heart damage and improve long-term prognosis.
Risk Factors for Mitral Regurgitation
Age and Gender
Mitral regurgitation risk factors can vary, with age and gender playing significant roles. The prevalence of mitral regurgitation tends to increase with age, particularly in individuals over 50. Gender can also influence the development of this condition, with men being more prone to acute mitral regurgitation, while women may develop chronic mitral regurgitation more frequently. Understanding these demographic factors can aid healthcare providers in assessing risk and implementing appropriate management strategies.
Other Medical Conditions
Various underlying medical conditions can contribute to the development of mitral regurgitation. These conditions may include a history of rheumatic fever, coronary artery disease, hypertension, or connective tissue disorders. Additionally, previous heart conditions such as myocardial infarction or heart valve abnormalities can increase the risk of mitral regurgitation. Identifying and addressing these comorbidities is crucial in the prevention and management of mitral regurgitation to improve patient outcomes and quality of life. Regular medical evaluations and diagnostic tests can help detect and monitor these risk factors, allowing for early intervention and appropriate treatment.
Complications of Mitral Regurgitation
Heart Failure
Untreated or severe mitral regurgitation can lead to complications such as heart failure. This occurs when the heart struggles to pump blood efficiently, causing symptoms like shortness of breath, fatigue, and swollen ankles. As the regurgitation worsens, the heart’s chambers may enlarge, weakening the muscle over time. Timely diagnosis and management are crucial in preventing the progression to heart failure.
Arrhythmias
Another complication associated with mitral regurgitation is the development of arrhythmias. Irregular heart rhythms can arise due to the heart’s structural changes resulting from the regurgitation. These abnormal heartbeats can lead to palpitations, dizziness, or even more severe consequences like stroke. Monitoring for arrhythmias through regular electrocardiograms and consultations with a cardiologist is essential for patients with mitral regurgitation to address these complications promptly. Early detection and appropriate treatment of arrhythmias can improve the patient’s overall prognosis and quality of life.
Also Read: Comprehensive Guide to Heart Valve Health: Symptoms
Treatment Options for Mitral Regurgitation
Medications
When it comes to the treatment of mitral regurgitation, medications play a crucial role in managing the condition. Patients may be prescribed medications like diuretics to reduce fluid buildup and ease the heart’s workload. Other drugs, such as ACE inhibitors or beta-blockers, can help in controlling blood pressure and improving heart function. It is important for individuals with mitral regurgitation to adhere to their medication regimen as prescribed by their healthcare provider to effectively manage the condition and prevent further complications.
Surgical Interventions
In cases where mitral regurgitation is severe or causing significant symptoms, surgical interventions may be necessary. Surgical options for treating mitral regurgitation include repairing or replacing the mitral valve. Valve repair is often preferred over valve replacement as it preserves the natural anatomy of the heart. Minimally invasive procedures may also be considered, leading to quicker recovery times and reduced postoperative discomfort. Consulting with a cardiac surgeon is vital in determining the most suitable surgical intervention based on the individual’s condition and overall health status.
