Introduction to Pelvic Pain
Definition and Overview
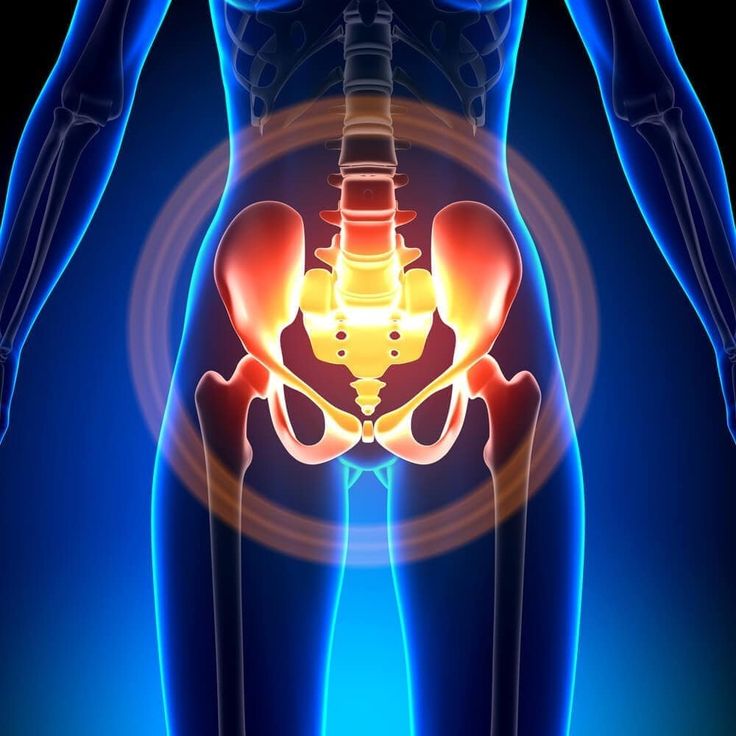
Pelvic pain is a common condition that can affect anyone, regardless of age or gender. It refers to pain or discomfort felt in the lower abdomen area, between the hip bones. This type of pain can be acute or chronic, sharp or dull, constant or intermittent. Understanding the underlying causes of pelvic pain is crucial in managing and treating this condition effectively. Consultation with a healthcare professional is essential for proper diagnosis and treatment options.
Common Causes
There are various reasons why individuals may experience pelvic pain. Common causes include menstrual cramps, urinary tract infections, bowel issues, endometriosis, fibroids, muscle spasms, pelvic inflammatory disease, and reproductive system disorders. In some cases, pelvic pain can also be a symptom of more serious conditions such as ovarian cysts, ectopic pregnancy, or pelvic organ prolapse. It is important to seek medical attention if you experience persistent or severe pelvic pain to rule out any underlying health concerns and receive appropriate care.
Types of Pelvic Pain
Gynecological Causes
Pelvic pain can stem from various gynecological issues. Conditions such as endometriosis, fibroids, pelvic inflammatory disease, and menstrual cramps are common culprits. Endometriosis occurs when tissue similar to the lining of the uterus grows outside it, causing severe pelvic pain. Fibroids, non-cancerous growths in the uterus, can lead to discomfort and heavy menstrual bleeding. Pelvic inflammatory disease, usually caused by sexually transmitted infections, can result in chronic pelvic pain if left untreated. Menstrual cramps, a common occurrence during menstruation, can also cause discomfort in the pelvic region.
Non-Gynecological Causes
Pelvic pain can also be caused by non-gynecological issues. Urinary tract infections, bowel problems, muscle spasms, and reproductive system disorders can all manifest as pelvic pain. Urinary tract infections can lead to pain and discomfort in the lower abdomen, while bowel issues like constipation or irritable bowel syndrome can cause similar symptoms. Muscle spasms can create sharp, cramp-like pains in the pelvic area. Reproductive system disorders such as ovarian cysts and ectopic pregnancy can also result in pelvic pain. Seeking medical advice is crucial to identify the root cause of pelvic pain for appropriate treatment.
Symptoms of Pelvic Pain
Common Signs to Watch For
When experiencing pelvic pain, there are common signs to watch for that may indicate an underlying issue. Persistent pain in the pelvic area, whether dull or sharp, could signal a gynecological or non-gynecological problem. Pain during intercourse or bowel movements is another common symptom that should not be ignored. Additionally, abnormal vaginal bleeding, unusual discharge, or fever accompanying pelvic pain may indicate a more serious condition.
When to Seek Medical Help
It is crucial to know when to seek medical help for pelvic pain. If the pain is severe, sudden, or accompanies symptoms like heavy bleeding, fainting, or severe abdominal tenderness, immediate medical attention is necessary. Persistent pelvic pain that disrupts daily activities or lasts for more than a few days should also prompt a visit to a healthcare provider. For women experiencing pelvic pain during pregnancy, medical evaluation is essential to ensure the safety of both mother and baby. Remember, early diagnosis and treatment are key to managing pelvic pain effectively.
Diagnosing Pelvic Pain
Medical History and Physical Examination
When diagnosing pelvic pain, healthcare providers typically start by taking a detailed medical history and performing a thorough physical examination. This helps to gather information about the individual’s symptoms, lifestyle, and any potential risk factors. The physical exam may include palpating the abdomen and pelvic area to check for any abnormalities or tenderness that could indicate the cause of the pain.
Imaging and Laboratory Tests
In some cases, healthcare professionals may recommend imaging tests such as ultrasounds, MRIs, or CT scans to get a clearer view of the pelvic organs and identify any issues like cysts, tumors, or abnormalities. Laboratory tests, including blood tests and urinalysis, may also be conducted to check for infections, hormonal imbalances, or other underlying conditions that could be causing the pelvic pain.Remember, accurate diagnosis is crucial for effective treatment and management of pelvic pain. If you are experiencing persistent or severe pelvic pain, it is important to consult with a healthcare provider for proper evaluation and care.
Also Read: Effective Pain Management Solutions for a Pain-Free Life
Treatment Options for Pelvic Pain
Medications
In treating pelvic pain, healthcare providers may prescribe various medications depending on the underlying cause. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation. For conditions like infections, antibiotics may be necessary. In cases of muscle spasms contributing to pelvic pain, muscle relaxants might be prescribed. It’s essential to follow the prescribed dosage and inform the healthcare provider of any allergies or side effects.
Physical Therapy
Physical therapy is often recommended as a treatment option for pelvic pain. It involves exercises to strengthen the pelvic floor muscles, improve flexibility, and reduce tension. Physical therapists can also educate individuals on posture, body mechanics, and relaxation techniques to alleviate pelvic pain. Additionally, techniques like massage therapy or acupuncture may be used to target specific areas of pain and provide relief. It is crucial to consult with a healthcare provider or therapist to develop a personalized physical therapy plan tailored to the individual’s needs and condition.
